Consider becoming a subscribing member. You get access to the weekly reading recommendations, the bi-monthly massive link posts, the knowledge that you’re paying for the things you find valuable….
Plus, you’d get access to this week’s really great threads — like yesterday’s full of ideas of what to actually watch when you sit down and say to yourself/your partner/your cat WHAT SHOULD WE WATCH?? and last Friday’s really fucking wonderful discussion of “What’s Your Favorite Part About Being Queer?”

A little more than a year ago, I wrote about my first colonoscopy. Most people think of colonoscopies as something you start doing when “you’re old,” but the new guidance is for everyone to get one starting at age 45. (I got mine at 40 because of family history — if you know your family, ask if you have history and get one done!) I wrote in detail about the prep, the facility, the procedure — I wanted to elucidate the process and make it less shadowy and intimidating. Since then, I’ve had a follow-up colonoscopy (even less dramatic the second time!) and I’ve heard from dozens of you who’ve also scheduled your own colonoscopies. THIS IS GREAT. MORE COLONOSCOPIES!!
But writing that piece reminded me of just how many medical procedures and conditions remain opaque. Like mammograms, colonoscopies are most often preventative (as in, you get one just to make sure nothing funny’s going on) but sometimes people get them because they’re in a lot of inexplicable pain — pain that others often chalk up to eating choices, age, body size, or stress.
Because of our various body taboos, it’s hard to talk about openly the way you’d talk about, oh, a headache — which means we often don’t talk about it at all, not even with a medical professional. Or if we do, like my friend Natalie did, it’s labeled psychosomatic (it was cancer).
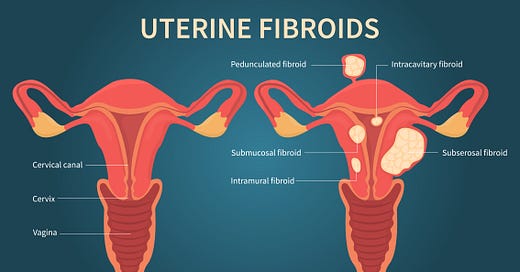
I’ve known a lot of people with severe menstrual pain — people who’ve been told, in various fashions, that it’s “normal” and “there’s nothing to be done.” As I’ve grown older, I’ve also known a lot of people who’ve been diagnosed with fibroids — usually only after pretty confusing and arduous medical journeys. Fibroids can develop when you’re younger; they can develop when you’re older; they can cause no pain or debilitating pain. 80% of people with uteruses develop them; 40% of those fibroids are symptomatic.
Many but not all people with fibroids have some sort of family history that may be obscured because it’s “not something we talk about.” Black people with uteruses are significantly more likely to develop fibroids and to start developing them at a younger age. (The reasons aren’t clear, but systematic racism in the health care system can also mean that they are less likely to have their symptoms and pain treated seriously).
If you have heavy and painful periods that make you question what’s “normal,” if you experience pain during intercourse, if you have weird poops or pelvic pain and/or lower back pain — read on, see if any of this sounds familiar, but most importantly, talk to your doctor, and if they brush it off, see if you can get a new one.
And even if you don’t have any of those symptoms, even if you don’t have a uterus, you should also read on — first, because it’s important to understand to bear witness to both the pain and bullshit that so many people have to go through to find relief, but also because there might be someone in your life (including yourself!) who has some of these symptoms someday. You don’t have to have the same health condition as someone else to provide solace and advocacy. Plus, we could also stand to be more empathetic about each other’s pain.
Finally: If you’ve dealt with fibroids in the past, if you’re dealing with them now: I hope this makes you feel even slightly less alone.
Just a heads up: These accounts include some graphic descriptions of fibroid symptoms. That doesn’t mean you should avoid them, just making that clear.
These stories have been edited very lightly for clarity and length.
Alycia, 45, Black, Cisgender Woman
My mother has fibroids. I'm sure there are more women in my family who do but there is no a culture of openly talking about this.
When I was 22 years old my period got super weird. I had just met my now-husband and was sexually active for the first time, but I was never pregnant. I would go several months without a period and then when it finally would come it was from hell. I remember going on a date where we took a one-hour ferry to a nearby island to ride bikes. From the time we got on the ferry to the time we arrived I completely soaked through my pad and had to change. At least once I had to stay home from work because the cramps were so bad. After a five month stretch when I hadn't gotten my period I went to see an endocrinologist.
I went to see a (young, white, male) endocrinologist with a handwritten timeline detailing my periods for the previous nine months. He asked me if anything had changed in my life in the past year and I said the only new thing was meeting my boyfriend. He said "Well, maybe that's it," gave me a prescription for birth control pills and sent me on my way. He never mentioned or asked about the possible existence of fibroids.
Ten years later, I got pregnant with my first child and the fibroid was visible on the ultrasound. It grew to about the size of a golf ball during that pregnancy. If I hadn't gotten pregnant I don't know if I ever would have known about it. It shrunk after that pregnancy and I have had an IUD in since my second child was born. I haven't needed treatment.
Roxy, 64, White, Cisgender Woman
I was post-menopausal when I found out about my fibroids. My periods had stopped completely at age 51 after being every other month for like 6 months. The last year or so was quite a bit heavier bleeding with some clots in it, so I was thankful to be done with it. I had some infrequent abdominal pain, but didn't think that much about it. I was working in a factory, and had worse physical pain than that to distract me. Then suddenly, six years later, I had a severe bleeding — like hemorrhaging — episode that absolutely terrified me. I was in the bathroom going pee, and went I went to wipe, there was a bunch of red blood.
I had to call off work, and because I had no pads or tampons anymore (I thought my period was over!) I had to fold up a huge bunch of paper towels to get to the store to get some pads. I had to keep changing the pads constantly, and I called the doctor as soon as I could. He did an exam, and tried to do a Pap (it didn't work — too much blood), but he told me I'd have to be referred to a specialist. The specialist I went to did an ultrasound, and that was when I was diagnosed with fibroids.
The diagnosis part was the easy part. There's no getting around what the ultrasound shows! I wish I could say that the specialist fixed the problem, but he didn't. I wanted a hysterectomy. He talked me into an endometrial ablation and D&C, and was supposed to remove the fibroids during these procedures (there were numerous). He did not. I had more trouble after this than before! More bleeding problems, pain, bloating. I went to a different doctor who re-did all the same tests and asked me why I didn't just opt for a hysterectomy? I explained, and he said he would be glad to schedule one for me. But the day my insurance approved the surgery I lost my job and my insurance.
I finally got my hysterectomy nearly two years later, but the doctor who performed it (a different one, because of different insurance) tried to talk me out of it. He couldn't or didn't believe I was in pain from the fibroids. The exam alone was torture. At the post-op visit, when he told me that the pathology report was non-cancerous, benign fibroids, he said my uterus was literally filled with them. I wanted to smack the shit out of him.
Anna, 36, Asian American, Non-Binary
Before my diagnosis, I had never heard of fibroids. I'd always had heavy periods, but I didn't think that was really out of the norm (and I guess "heavy" is kind of subjective). At some point, I noticed my periods were getting heavier (on the first couple of days, I would soak super heavy pads approximately every 45 minutes) and I brought it up with my doctor. She ordered an ultrasound, and that’s when I discovered I had one about the size of a grapefruit.
I never had to convince my doctor something was wrong with me. I didn't even know that my heavy periods were not "normal" until I described it to her and she totally took the initiative to check for any abnormalities. Once diagnosed, she walked me through my options (leave it alone vs. surgery and the different types of surgery) and advised me based on my situation. Since my fibroid wasn't causing me any pain, I was put on the pill to see if it would lighten up my periods. For a time it helped, but after a few years, my period became even heavier; at one point, I fainted due to how much blood I was losing. I made the decision then to have surgery.
Ideally, everyone would have as good of an experience as I did: a doctor who listened to my concerns, ran tests to check, continually monitored status of fibroid, talked to me several times about my options and gave advice without ever pushing any particular treatment.
See, 39, Chinese/Singaporean
I had excessive flow and random spurts of bleeding outside the normal period. It was freaky, as I really didn’t know what the cause was and it would bleed a ton when I jogged, which I did several times a week.
Turned out it was a 2.5cm submucosal fibroid (a bad kind of fibroid that gets symptomatic — not all are) that my uterus had somehow pushed down into my cervix. I had it taken out via a hysteroscopy — it was a day procedure, and I had such a good break from work. My doctor was professional and above board. But then again, I don’t live in the United States.
Margaret, 35, Mixed Race (Black + White), Cisgender Woman
My IUD strings were no longer visible outside of my cervix and I had a transvaginal ultrasound to confirm that the IUD was still in place. That was when I first learned that I had a 3-4 cm fibroid. I later found out that the issue with my IUD strings can be caused by fibroids, but my doctor didn’t make the connection at the time.
Over the next two years ago I began to have constant pelvic pain, sometimes shooting, sometimes like a deep ache not dissimilar from period cramps. I was also having “bulk symptoms” due to the increasing size and location of my fibroid; it hurt to wear tight or rigid pants and if I sat down too hard it was like a lightning bolt up my spine. My periods got heavier and longer until I was afraid to leave the house for a couple of days each cycle because I would soak through a pad and a tampon within 30 minutes.
When I was first diagnosed by happenstance during an unrelated ultrasound, I wasn’t given much information about fibroids or the symptoms they can cause. I was told not to worry about it, basically. Once I started having pretty severe symptoms a couple of years later I went to see a different gynecologist. I learned from her that my fibroid had already grown to 7+ cm which eliminated the possibility of non-surgical options for removal. I wish I had known earlier what symptoms I should be watching for and what treatment options were available at an earlier stage in my fibroid’s growth.
After my gynecologist informed me that surgery was my only option, I was referred to a surgeon for a consultation about myomectomy (surgical removal of the fibroid). He insisted that an open procedure was my only option due to the size and location of my fibroid, which would require a multi-month recovery. This surgeon boasted to me about how he had performed the same surgery on his wife and sister-in-law, and assured me that “the only person who will be able to see your scar is your husband.” He was adamant that, without removal of this fibroid, I would never be able to carry a pregnancy to term.
I had a terrible feeling about that first surgeon I saw. I also felt under-informed about the fertility implications of removing or not removing my fibroid. I don’t yet have children but am fairly certain I would like to have them in the future. Thankfully, a friend of mine was going through fertility treatment at the time and recommended her doctor to me for a consultation. Even more thankfully, the company I worked for at the time offered a fertility benefit that would reimburse 80% of the cost of that consultation (which was not covered by my medical insurance).
I learned from the fertility specialist that I could likely conceive with my fibroid in place, but that the fibroid would continue to grow during the pregnancy and would likely cause me a lot of pain. It could result in early labor or miscarriage. I also learned that many women have successful pregnancies after undergoing a myomectomy, but that I would need to deliver via c-section.
The fertility specialist referred me to a different surgeon who was shocked that I had previously been recommended for open abdominal surgery. She performed a successful laparoscopic myomectomy, removing my jumbo fibroid and 2 smaller fibroids that weren’t visible on ultrasound. The surgery entailed a 4-week absence from work and a pretty seamless recovery and I feel approximately a million times better now that my fibroid has been removed. I can’t recommend Dr. Kristen Pepin at Weill Cornell enough to anyone else needing minimally invasive gynecologic surgery in the NYC area.
See your gynecologist! Ask them about their experience with fibroids. If they don’t have much info to offer or disregard your symptoms, seek out a doctor who specializes in fibroids. If possible, I would also suggest learning about your family members’ experiences with fibroids — in my experience sharing family history with medical professionals can help get your case taken more seriously. (My paternal grandmother had a fibroid the size of a football removed in her 60s)
Knowing what I know now, it’s wild to me that fibroids aren’t included in our definition of preventive gynecological care, especially for the most at-risk populations. Earlier screening and monitoring likely would have saved me thousands of dollars and unquantifiable pain & suffering. And even though I know that my fibroids might return someday after surgery, the procedure was 100% worth it for me. It was scary to go under the knife but I can’t even describe the improvement to my quality of life. I wasn’t really aware of how much pain I was in until it was gone.
Kelly, 50, White, Cisgender Woman
I had heavy periods, but just thought it was part of aging. I remember my mom having extremely heavy periods as she aged and figured it was just how it went. But then I was trying to get pregnant and it wasn't working. After blood tests and all that, I was sent for an ultrasound where they diagnosed me with numerous fibroids.
The gynecologist was the one that told me I probably wouldn't get pregnant unless I had them removed. She was very kind and helpful, but then again I was already past the general practitioner at this point. I'm Canadian. Everything was covered completely.
Sojourna, Black, Cisgender Woman
The symptoms were subtle but looking back it was obvious. My periods were bad for about a year, to the point where I had to set an alarm for the middle of the night to make sure to change my pad. I developed iron deficient anemia and my energy levels went down. I put on weight seemingly overnight and developed sciatica pain. One night I was doing yoga and did an exercise that involved me pushing down on my abdomen. I felt a growth and it all snapped into place.
I had a really good relationship with my doctor but had bad insurance. I didn’t want children and she already knew that. She went over my options, but at the time I was interviewing for new jobs out of state. I got a new job, moved and immediately went to a doctor with the goal of a UFE [Uterine fibroid embolization]. The immediate reaction of “obviously you want children so a UFE is out of the question” was offputting because of my previous relationship with my doctor. I had to tell her want I wanted very clearly but once she heard me, the process went quickly.
I was shocked because for a long time I had really bad insurance. I moved in July, visited the doctor in August and planned a procedure for January because I thought I needed time to pay for it. I got preappoval from my insurance, ran numbers and couldn’t get a clear answer on costs. But I prepped for about $3000 out of pocket. About a month after the procedure I got a bill for $80 and thought about how shitty it was that so much of our livelihood is tied up with our job based insurance. When I didn’t have the money, I couldn’t afford it. When I had the money, it became affordable.
I was lucky — my mother prepared me for what happened because of her history with fibroids. But also: so many Black women in my life had them. Once I mentioned them in conversation, my friends came out and talked about their problems with them. One of my friends had disappeared for about a month the year before — turns out she had a hysterectomy.
I’m still in the process of healing from my UFE (it takes 6 months for the fibroids to shrink) but the changes were immediate. My back and leg pain ended and my cramps became bearable. The White Dress Project is also doing really good work explaining symptoms and options, it’s one of the first places I would send people.
People should also know that a hysterectomy/myomectomy isn’t the only option. That’s the option doctors push because it’s within their comfort level. Black women are often pushed because doctors have this idea of what’s best for them. But this should be a decision with multiple options, not just one.
Sydni, 24, Mixed (White and Métis), Cisgender Woman
I got my period for the first time at 11, and they were always heavy and very irregular: one time I bled for 28 days straight. I went on the combined pill around age 13 and took it for a decade with no problems; my periods were still heavy, and very painful for a day or two, but very predictable and otherwise fine.
When I moved from Canada to Scotland for grad school in 2021, my new GP switched me to the mini pill (progesterone only), because in the UK they don't prescribe the combined pill to migraine sufferers (increased blood clot risk). This was slightly alarming — I'd been a migraine sufferer at home too, but okay, I guess?! I was told to expect that my periods might stop, but they could come back after a few months, or not!
Six months after going off the pill (and moving to England), my period still hadn't come back, and I was getting increasingly concerned and bothered. I want to get pregnant in the next five years or so, and as a historian of motherhood, it's on my mind constantly and deeply entwined with my work. I miss having a period; for all its inconveniences it was predictable, and I could map my moods, libido, and physical symptoms (back pain, acne) neatly onto a hormonal cycle. I wanted that back, even though (as a lesbian dating another cis woman) fertility wasn't something I actively needed to be monitoring just yet.
I got bloodwork done through a private online startup (Hertility) and the results showed that I might have PCOS, which I hadn't been expecting. I was initially very skeptical — I thought the irregular periods had more to do with the pill, and possibly even my Crohn's medication, than with my ovaries themselves, especially as I didn't have any of the other hallmarks, like hirsutism.I brought the results to my GP, who did more bloods and sent me for a pelvic ultrasound. She then performed a transvaginal scan, which revealed a small and apparently well-behaved fibroid. I don't have a family history of fibroids so I did some research and found that this, as well as the tipped uterus, could definitely be responsible for the lower back pain (generally present but excruciating during periods), pain during penetrative sex in certain positions, and heavy menstrual bleeding.
I find the GP system in the UK utterly baffling. Whereas in Canada I could book doctor's appointments weeks, months, or even a year in advance, in the UK I have to call in at 8 a.m. and hope to be allotted one of today's available slots. If I don't manage it, I have to try again tomorrow. For someone with a chronic condition (now possibly two), this results in a huge amount of time, energy, and frustration spent on managing just the administrative portion of my illness(es), to say nothing of the symptoms themselves. I am fortunate, as a PhD student with no care dependents, to be able to make my schedule work for this, but not everyone has that privilege.
I wish I'd known as a very young teen that my heavy, painful periods had a named cause and weren't just "how it's going to be." Also, the birth control pill has been an excellent choice for me, but it's definitely not for everyone! Giving people choices in their reproductive health, instead of just prescribing a one-size-fits-all solution without question, is hugely important. Young people have bodily autonomy too.
Heather, Mid-Forties, White, Cisgender Woman
I knew something was wrong pretty quickly. My periods had always been mercifully short, light and pain free. I never had to use more than the "regular" pads and tampons. Then suddenly I had terrible cramps, periods that were lasting weeks, and I was passing huge amounts of gloppy, clotty gunk.
At first I listened too much to friends and acquaintances who assumed I was just hitting menopause age and experiencing "flooding" and this was "normal." Once I went to my OB-GYN, who's pretty great and no-nonsense, she diagnosed me right away and confirmed it with a ultrasound. Getting the problem to actually stop took years. Birth control meds slowed down the bleeding for a little bit. Then we tried just removing the fibroids in a simple surgery (which was my first "real" surgery, so a scary experience for me). That worked for about 2 years, but then they grew back worse than ever. I couldn't leave the house many days due to cramping and constant bleeding, and I developed anemia after a 90 day long period. After discussing it with my doctor and getting a few second opinions, I eventually had a robot-assisted laparoscopic hysterectomy. When they looked at my uterus after removal they said there was one large fibroid the size of a lemon that was "pumping out blood" and over 10 smaller ones.
I was very lucky and had very good health insurance and access to state disability insurance through my job when I had both my surgeries. My salary was paid through the time I was off and most of my medical expenses were covered. I still ended up owning about $2500 per surgery in medical expenses from copays, co-insurance, blood tests, and other fees. I have no idea how a working mother without good insurance could have managed it.
Lena, 44, Latina, Cisgender Woman
I always had long (a full week of bleeding) and heavy (using super tampons and overnight pads for the first several days) periods since I got my period at age 11. My periods got heavier (needing to change super tampons every hour or two) sometime after I turned 40, but I assumed it was just a normal perimenopause thing. I was eventually diagnosed after routine bloodwork during a physical showed I had super low iron levels.
My primary care provider referred me to a hematologist. He asked about my periods and said that was often a cause of iron deficiency, and referred me back to my PCP. She prescribed birth control pills, which made me bleed continuously for a few months. In the meantime, the hematologist ordered blood transfusions. When there was no improvement, he recommended follow up with a gynecologist. She did a vaginal ultrasound, diagnosed fibroids, and recommended surgery and an IUD implantation.
I was incredibly lucky. All of my doctors (PCP, hematologist, gynecologist) had low copays ($10) and there was no cost for the iron infusions (billed at $1500 each; I had 3 cycles of 3 infusions each). The surgery was out patient; my total out of pocket was $500 (the total billed was about $30,000). The total billed for all of the visits and treatments was $44,000; I paid $560.
My gynecologist told me that people often don't know what normal or abnormal flow is, since mostly they only know their own experiences or maybe their family members' (who may have similar problems). Asking patients about their periods and talking about what is not normal would keep more people from suffering unnecessarily.
Mary, 30, White, Cisgender Woman
My fibroids actually didn't lead to an abnormal period. I had totally normal periods (and still do), but I have insane pelvic pain upon arousal. My husband is a doctor (not an OB, though) and felt around after a few attempts at sex were cut short by the pain. He felt a lump, said "I bet that's a fibroid!" and made me go to an OBGYN. The OBGYN felt a lump, got me an ultrasound and MRI, found a fibroid and an ovarian cyst (lucky me!). They said basically it's too small to worry about but we'll keep checking on it yearly and there's nothing I can do about the pain.
I'm lucky. Husband knew what it was and my oB felt it right away. No race or size discrimination or doctor switching yet, though i am considering a second opinion about anything i can do about the pain.
Reighan, 42, African American/Black, Cisgender Woman
My periods were really heavy. They had just grown steadily heavier — so heavy that I would bleed through a pad and tampon in like 30 minutes.
I went to a medical professional at the campus student health facility. The person was a white woman. She thought I should get tested for an STD and iron deficiency. When neither came back positive I heard nothing else. I indicate the race of the woman because I think she fit me into a stereotype of possible sexual promiscuity. I continued with the heavy periods until I went to an Asian American gynecologist who felt something and sent me for tests. I'm grateful to her. Another Black woman recommended the Asian American woman doctor to me because of her care. I then went to a white male fibroid specialist and he told me to just leave it. Then I moved to LA and went to a Latina fibroid specialist. She was the best. We talked about my options and she recommended surgery. I had a myomyectomy that was laproscopic due to her expertise.
There are groups on Facebook that I've found to be helpful. People share information about doctors and surgeons they've found to be helpful. People make recommendations and share experiences about healing after surgery. They share pictures of their babies they had after having fibroids removed. Spaces of camaraderie and sharing can be important forms of community and knowledge when dealing with these health issues.
Sherri, 55, White, Cisgender Woman
The first time I was diagnosed, I was around the age of 35 or 36. I've never had a "normal" period. They were never monthly and never the same flow. Once I got on the pill (around age 17), that helped regulate them happening monthly, and at first, it helped regulate the flow. Over the years, that changed, but that change happened slowly. Around the age of 33 or 34, my periods started becoming so heavy and painful that they affected my work, so I spoke to my OB/GYN about what I was experiencing. She said it was normal for periods to change and that I should try a different form of birth control pill. So I did. And then I tried another and another. Nothing worked, and at no time did my female OB/GYN mention fibroids or ask if there was a history of them in my family. I should note, though, that my mom is very bad at discussing family medical history. It wasn't until I had surgery scheduled that she told me she had also had them and had had a hysterectomy because of them. I resigned myself to losing two weeks of my life every month to dealing with PMS and then heavy bleeding.
It took getting a new primary care doctor who took my symptoms seriously and then getting a new OB/GYN to confirm it. I don't think it was a language thing, I wasn't saying anything in a new way. I honestly think it just took finding a doctor who didn't think that heavy periods are just a thing women have to deal with.
H, 35, half Mexican/half white, Masculine Butch Lesbian
My periods have been heavy for a very long time, but in 2021 I started having extremely frequent spotting that became disruptive, and felt a mass in my abdomen that seemed to be growing.
I went to a new gyno who refused to ultrasound me. She insisted the mass I felt was a tilted uterus. At the time I was poly, and she was much more fixated on the fact that I had 3 partners and made comments about how that wasn’t “safe,” and that the spotting was probably from getting scratched while getting penetrated, which felt ludicrous to me given the amount of blood I was losing (and I was only having sex about 1-2 times a week). I ended up going back and insisting on an ultrasound, and she reluctantly did, then seemed to feel guilty when she noticed at least four masses inside. I changed doctors and got a more advanced ultrasound which showed six masses, two of which were about 7 cm in length.
My new doctor wasn’t receptive to the questions I asked about getting a hysterectomy. I explained I had no intention of carrying a child, but her pushback seemed oriented around wanting me to keep the option open. She said she would refer me to a surgery consult only if I tried other options first, such as a hormonal IUD. I didn’t love the idea but felt pressured into it. When I returned for the IUD insertion, she held my cervix open and tried to get the IUD in for about 10 grueling minutes while I cried and bled all over the table. She finally gave up and explained that the largest fibroid was preventing it from going in. She seemed to feel bad, apologized and left. I messaged her through my health portal a week later asking for a surgery consult again, but she wanted me to try a 6-8 month regimen of Lupron instead — injections that would put me in temporary menopause with a ton of side effects that sounded awful. I gave up.
In more recent times, my now monogamous partner and I decided I would do an IVF egg retrieval for a child she wants to carry next year. We decided that I would go for a hysto after that with a new doctor, especially because I had been experiencing more intense quality of life symptoms from the fibroids that felt like estrogen dominance and extremely horrible PMS. Our fertility doc has been awesome. She noted that my fibroids have grown even more, and validated that hysterectomy is my only way out. I’ve just finished my egg retrieval in the last week — a harrowing hormonal nightmare, honestly — and the massive amounts of estrogen throughout caused my fibroids to grow a noticeable and alarming amount. The largest one now feels like the size of a small football and juts completely out of me, causing a noticeable disfiguration to my profile and feels really uncomfortable. I’m still waiting to meet with my new doctor to learn more about next steps and hoping she’s receptive to my desired plan.
If a friend came to me and thought they had fibroids, I’d tell them to go to their OBGYN and absolutely insist on an ultrasound. I’d also tell them to exercise caution with the lesser interventions that could be prescribed. I’ve had friends with just 1-2 small fibroids have success with a myomectomy, but I think for cases like mine that are more moderate/severe, more drastic surgery is probably the better option. I’ve read a lot of anecdotes from women who feel immense relief after getting hystos, and I’m looking forward to that myself.
Tej, 30, Indian, Cisgender Woman
Both my mother and aunt have fibroids, but I’ve never had any indications. I went to have an ultrasound sonography for PCOD (Polycystic Ovarian Disease) and the pathologist pointed out their existence. I didn’t have to change doctors. Mine offered several options and explained the consequences. We decided to wait to see if they shrink on their own, and not try hormonal meds or surgery, because I have no other symptoms or effects. The size has remained the same over a period of one year. But I have do have to keep close watch and have an ultrasound every six months to check progress — especially before planning a pregnancy.
Leslye, 45, Black, Cisgender Woman
My mother had fibroids, and I’m pretty sure about all the women in my family have as well. I had incredible pain with my ovulation starting in my mid-twenties, but I didn't realize what it was from for a very long time. In my late 20s to 30s I began experiencing longer and more painful periods; at one point, I was spotting for about two weeks a month, and my cramps were so bad they would put me in the ground in the fetal position. At around 30, my stomach started getting bigger until I began to look pregnant and knew I had fibroids.
I waited a long time to go to the doctor, so as soon a I lifted up my shirt, the doctor was like, yes you have fibroids. At 32, I had my first myomectomy surgery to remove the fibroids. It was covered by my insurance. Since I'm self-employed, I had a large deductible plan, so I had to pay quite a bit to cover it. But otherwise, everything was covered.
I ended up needing a hysterectomy at age 38 because I had adenomyosis. I'm not sure if that's related to the fibroids or not. As a childfree woman, it's been difficult having my choices taken away like that, but my hysterectomy was the best thing that's ever happened to me. I have such freedom now, from my period and the pain that came every month.
Caty, 49, White, Cisgender Woman
This is all super fresh for me as I was just finally diagnosed last week. My period had been sporadic for last two years and I thought I was well on my way to full menopause. I started on bio identical hormones a year ago and had a vaginal Ultrasound prior to starting that treatment and everything was clear. Then I started having my period again and then I started bleeding heavily and it didn’t stop for a full month.
My issue was two fold: 1. as a lifelong lesbian, I did the least in terms of reproductive care (basically Pap smears as suggested by my (male) GP) so I never had a personal gynecologist. 2. It was hard to schedule any kind of appointments or tests at the crest of Omicron in my city. I finally got an appointment for vaginal ultrasound, and it went smoothly, but it took ten days for my doctor to find time to bring me through findings and diagnosis. I’ve got 4 fibroids, the largest is the size of a kumquat (why growths are always described in relation to fruit I will never understand).
While on the phone with my doctor, my fiancé actually grabbed the phone out of my hand and described all of my symptoms (especially psychological ones) in a way I didn’t have language for. We decided best treatment option at my age is endometrial ablation (which basically ensures a baby would never be carried to term) but I am still trying to schedule treatment.
Anu, 32, South Asian, Cisgender Woman
Here really is the core of it: that I had no idea, and yet really, I had some idea. I found out, after a year of trying to get pregnant, that I had three giant tumours spreading across the entire width and height of my uterus. The MRI imaging was shocking: my actual uterus was squished in a corner while this giant, blood-filled sac took up half my body. While I was disappointed and worried that the myomectomy could result in more fertility issues, I felt weirdly vindicated. I sent the MRI image out to friends and family WhatsApp groups to say: LOOK I wasn't making it up! I finally had a reason: for being so tired all the time, for preferring to lay down with a heating pad on my abdomen for half the day, for feeling lazy/depressed/fatigued all the time. I thought I was exaggerating the painful periods, or that the "pain" and discomfort I felt was psychosomatic and mainly just in my head.
It took me a very long time to understand exactly what was going on and why. I was sent from a fertility clinic, where I had a ton of tests (HSG, transvaginal ultrasound, blood tests) to a specialist OBGYN clinic that had me do an intensive pelvic MRI. It also just felt like I lost trust in and connection with my body. I found out after the surgery that the doctors removed the equivalent of 2/3rds of my uterus. I really don't know if I'll be able to get pregnant after I heal. It's been about four months since the surgery, and I'm filling laying on the couch right now with a heating pad on my stomach. It's shit. I feel pain and discomfort but, again, I kinda feel like maybe it's in my head?
I was on grad student insurance when I was diagnosed, but even with coverage (that ended a month after the surgery), I ended up spending $7000 just for the myomectomy. This doesn't even cover the thousands on all the diagnostic tests. Even now, I'm worried about going back to my doctor for the pain I'm feeling. Is it bad enough pain to spend $100 just to go sit in a room and tell her I feel bad?
Thank you beyond words to the hundreds of people who shared their fibroid stories with me — I read each and every one, and wish I could’ve included them all.
You can find so many more fibroid resources at The White Dress Project. and check Alanna Okun’s excellent illustrated essay on the diagnosis and healing process.
If you enjoyed that, if it made you think, if you *value* this work — consider subscribing:
Subscribing gives you access to the weekly discussion threads, which are so weirdly addictive, moving, and soothing. It’s also how you’ll get the Weekly Subscriber-Only Links Round-Up, including the Just Trust Me. Plus it’s a very simple way to show that you value the work that goes into creating this newsletter every week!
As always, if you are a contingent worker or un- or under-employed, just email and I’ll give you a free subscription, no questions asked. If you’d like to underwrite one of those subscriptions, you can donate one here.
If you’re reading this in your inbox, you can find a shareable version online here. You can follow me on Twitter here, and Instagram here — and you can always reach me at annehelenpetersen@gmail.com.



Thank you. I am a queer woman diagnosed with fibroids at 37 when my spouse and I went to a fertility clinic to try to get me pregnant. I'll leave out the rest of demographic info for an attempt at semi-privacy given the details here.
1. I went to five gynecologists in a two-year period (2 fertility specialists, 2 regular gynecologists, 1 gynecological surgeon). The only one whose treatments and choices didn't actively worsen the situation was the surgeon.
2. I'd been sick for much longer than I knew. The level of bleeding I'd experienced since I first began menstruating was never normal or safe. My anemia was becoming disabling by this point and it's probably a good thing I bothered going to the fertility specialist. Even though her prescriptions and choices made the whole thing worse.
3. The surgeon was willing to support my fertility choices, and therefore did a myomectomy to remove the fibroids. Turned out, however, there were a lot of them. She removed thirty, the largest being cantaloupe-sized. Recovery was very difficult.
4. Unfortunately by the time I went for another fertility check-in (with a different doctor since the first was so damaging), there was a new large and rapidly growing fibroid. Childbirth was out of the question and the new fibroid was placed in a way that caused new, exciting, and different disabling symptoms. I went back to the surgeon, who prescribed Lupron to shrink it so she could do minimally invasive hysterectomy.
5. Lupron medical menopause is the worst. The mood swings and the body changes and the hot flashes!
6. I felt so much healthier after the hysterectomy. Not being anemic, priceless.
7. Years later, I am now undergoing what I believe to be early menopause (hard to tell, since I don't menstruate, but I have a number of other symptoms), likely triggered by ovarian damage from the two surgeries. The surgeon had to cut around scar tissue from surgery #1 to save the ovaries in surgery #2.
8. I might have found out about all of this earlier except that I hadn't been to gynecologists for several years... because I had severe pain with every pap smear... because there was a fibroid sitting on my cervix, and my previous gyns did not notice this. I thought I was a wimp who couldn't handle normal tests. None of my gyns acknowledged the pain or gave me ways to deal with it.
9. I do not, and will not, have children. A lot of the journey involved accepting infertility.
Thank you for collecting these stories, AHP.
Thanks for creating and sharing this piece. I am a woman who struggled with a variety of symptoms that impacted my life on a daily basis for years and years, and was told by every single doctor I saw that it was absolutely simply “anxiety”. It wasn’t until my gastrointestinal symptoms because so extreme that I saw a new GI doctor who finally recommended a colonoscopy at age 29 that it was discovered that no, I didn’t simply have anxiety — what I actually had was a tumor so deadly it is referred to in the literature as the “ticking time bomb tumor” because it will, if undiscovered, eventually just give you a stroke one day and kill you. Two days after I turned 30, I had the tumor removed. It was a harrowing surgery and recovery (full abdominal incision from belly button to sternum), but all my symptoms dissipated pretty much immediately.